Dr Soo Jung and colleagues (Seoul National University College of Medicine, South Korea) included patients with a renal score of at least 8, comparing robot-assisted partial nephrectomy (RAPN) (n=336) to open partial nephrectomy (OPN) (n=372) in complex renal tumours. Operating times were somewhat faster in the robot-assisted arm, suggesting that they were highly experienced surgeons. The authors saw significant improvements in post-operative pain and median length of hospital stay; however, there was no benefit with regard to the complication rate. Given that a few trials have reported a reduction of complication rates with RAPN [1], the value of RAPN still needs to be determined. This topic will also be investigated in a study by Prof. Arnulf Stenzl (University of Tübingen Medical School, Germany) and Prof. Marc-Oliver Grimm (Universitätsklinikum Jena, Germany) in a randomised prospective multicentre trial (20 centres, OpeRA study) aiming to compare RAPN vs OPN in patients with a renal score ≥7. A total of 606 patients will be monitored at 30 days and 90 days post-nephrectomy and the patients will receive a number of questionnaires regarding pain, recovery, and quality of life. The primary endpoint is the complication rate, and it is anticipated that this study will conclusively address whether RAPN is associated with fewer complications compared to OPN.
Enhanced recovery after surgery may significantly reduce length of hospital stay without compromising safety.
Better known from cystectomies and prostatectomies, Dr John Withington et al. (Royal Free London NHS Trust, UK) analysed enhanced recovery after surgery (ERAS) for nephrectomies following a diagnosis of renal cell carcinoma. The ERAS program starts at referral and ends with discharge. The patients and nurses have checklists, so everything is very well structured and pre-defined. The results from this study indicated that the complication rates were similar, but the length of stay could be halved by this structured approach. The re-admission rate was even reduced in the post-ERAS period and patient satisfaction was maintained. One potential bias the authors investigated was that RAPN was more likely to be performed in the post-ERAS period and in a multivariate analysis, they confirmed that the largest impact on length of stay was indeed ERAS itself and not RAPN. So, this is an opportunity to reduce length of hospital stay.
Neoadjuvant treatment may facilitate partial nephrectomy.
In a prospective randomised trial from Dr Oleg Voylenko (Kiev Medical University, Ukraine), 58 patients received 2 cycles of pazopanib prior to scheduled surgery, and 60 patients surgery only. Baseline parameters were balanced between groups, with tumour size averaging 61 mm in the control group, and 63 mm in the neoadjuvant group. In the neoadjuvant group, 86% of the patients manifested some tumour size decrease (average decrease was 12 mm or 20% of the tumour volume); however, there was less shrinkage in high-grade disease. No patient had progressive disease. The surgeons were able to perform a partial nephrectomy in 91% of the cases that had received neoadjuvant pazopanib, compared to only 33% of the patients in the arm that proceeded directly to surgery (see Figure).
Figure: Type of surgery for neoadjuvant targeted therapy vs surgery only for localised RCC
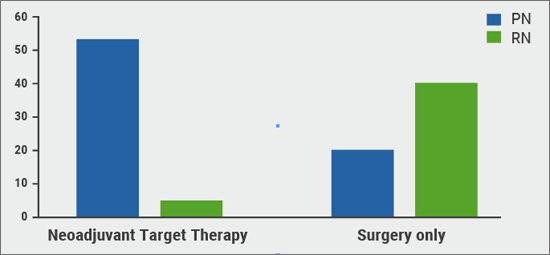
In the group of patients receiving 2 rounds of neoadjuvant targeted therapy (TT; N=58), 91% were able to undergo partial nephrectomy (PN). In the surgery-only group, 66% of the patients had to undergo radical nephrectomy (RN). RCC, renal cell carcinoma.
Positive surgical margin is an independent predictor of recurrence-free survival.
Dr Aaron Bradshaw (University of California San Diego, USA) and colleagues studied the impact of positive surgical margins (PSM) in a retrospective multi-centre analysis (n=2,737) undergoing partial nephrectomy (cT1a 1842 and cT1b 774). With a median follow-up time of 44 months, there was a PSM in 4.3% of patients (n=113). Using multivariate and univariate analyses, the authors demonstrated that PSM was an independent predictor of recurrence-free survival (HR 2.8, P<0.01). The authors also concluded that patients with cT1b tumours are at increased risk of recurrence and mortality and require a closer follow-up or even a secondary nephrectomy.
No apparent benefit of partial nephrectomy over radical nephrectomy in young (<50 years) and healthy patients.
Dr Hung-Jui Tan (University of North Carolina at Chapel Hill, USA) et al. considered the outcome after partial nephrectomy vs radical nephrectomy in the young (<50 years) healthy patient in the US National Cancer Database. Median age of this cohort was 44 years, and included 2,454 radical nephrectomies and 555 partial nephrectomies (18.4%) with a long median follow-up of 109 months. No differences in long-term overall survival between the two groups was observed (weighted HR 0.83, P=0.196). The authors conclude that, assuming familial tumour syndromes have been excluded, there is no need to take an oncological risk in the young and healthy patient with highly complex tumours. The patients have enough functional reserve; the advantage of partial nephrectomy in these patients has to be carefully questioned.
Pancreatectomy is an option in selected patients with oligometastatic disease.
Dr Steven Rodgers et al. (Sylvester Comprehensive Cancer Center, USA) performed a systematic review of 31 non-randomised studies, totalling 566 patients to examine the role of pancreatic metastasectomy for advanced renal cell carcinoma. The median age at pancreatic resection was 63.9 years. Most patients were metachronous (87.6%, vs 12.4% synchronous) after a median disease-free interval following primary resection between 40-160 months. Recurrence in the pancreas is usually late. The median overall survival in the various studies was between 15-148 months. The median disease-free survival was notably long at 34 months; these data support the notion that pancreatectomy might offer a good opportunity to manage disease for long-term remission. The overall operative morbidity, however, was high (13-57%), with 4.5% perioperative mortality. The conclusion of this systematic review is that there may be benefits for selected renal cell carcinoma patients with pancreatic metastases but there is a substantial perioperative risk.
New strategies/more research needed to optimise follow-up in curative surgery for RCC.
Dr Saeed Dabestani (Lund University, Sweden) examined image-based follow-up after surgery, using results from a multicentre database (RECUR). Imaging intensity was studied with regard to outcome after disease detection in 1,612 patients with 17,333 imaging procedures analysed. A total of 336 recurrences were observed. Overall survival did not improve for patients for whom more than twice the number of imaging procedures were performed than recommended by the EAU guidelines. Interestingly, patients who received fewer procedures than recommended by the EAU guidelines had nearly identical OS curves as well (see Figure). It is of note that per patient treated for recurrence and remaining tumour-free after treatment, 542 imaging procedures were required (in high-risk patients, 697). In short, there was no survival benefit associated with additional imaging procedures.
Figure: RCC overall survival after recurrence detection, stratified by imaging ratio
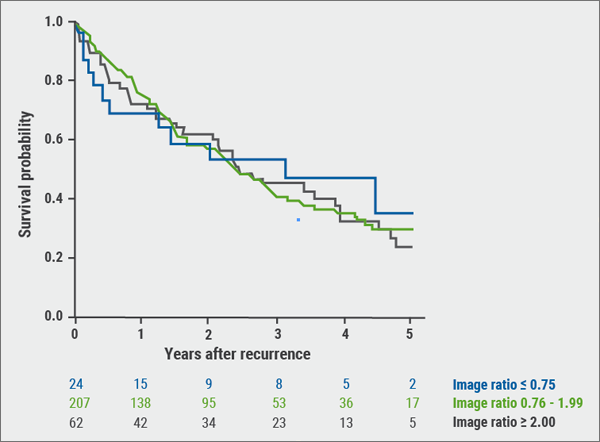
Image ratios defined as total number of imaging divided by estimated number of imaging for the given follow-up period according to the 2017 EAU guidelines follow-up imaging recommendations. No statistically significant difference between the groups was demonstrated. RCC, renal cell carcinoma. Kindly provided by Dr Dabestani
Posted on
Previous Article
« Skin and nipple sparing surgery: still a matter of debate Next Article
Testosterone replacement therapy: Safe and maybe even protective »
« Skin and nipple sparing surgery: still a matter of debate Next Article
Testosterone replacement therapy: Safe and maybe even protective »
Table of Contents: EAU 2019
Featured articles
Prostate Cancer
Barentsz Trial – Bi-parametric MRI versus multi-parametric MRI
Enzalutamide plus ADT improves outcomes for metastatic hormone-sensitive prostate cancer
Prostate cancer active surveillance: Better patient risk stratification and use of imaging
The role of pelvic lymph node dissection in prostate cancer: Extended vs standard
When to use imaging and imaging-guided therapies
Radioguided surgery is the future?
Bladder Cancer
Largest safety study of its kind with atezolizumab in metastatic bladder cancer
Bladder cancer risk and early detection
Consensus treatment pathway for patients with limited pelvic lymph node involvement in otherwise localised bladder cancer
FGFR3 gene mutation: Favourable prognostic impact in bladder cancer
Bladder cancer in young patients
Spanish study directly links surgical volume with mortality in bladder cancer patients undergoing cystectomy
Updated interim results of phase 2 trial of pembrolizumab for high-risk NMIBC unresponsive to BCG
Robot-assisted radical cystectomy or open radical cystectomy?
Renal Transplantation and Renal Cell Carcinoma
Andrology
Microdissection testicular sperm extraction (microTESE)
Male infertility/Premature ejaculation
Testosterone replacement therapy: Safe and maybe even protective
Focus on treatment of erectile dysfunction and Peyronie’s disease
Penile prosthesis implantation
Functional Urology
Decision aids are too difficult for patients
Lower Urinary Tract Symptoms
The Urodynamics for Prostate Surgery Trial
Minimally invasive surgical techniques must compete against pharmacotherapy in benign prostate hyperplasia (BPH)
Related Articles
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy

