Knowledge of bladder cancer was tested in the French population through the EDIFICE 6 study which surveyed >12,000 individuals online with no history of cancer. The cohort was demographically validated as a representative cross section of the French population (Dr Thibault De La Motte Rouge, Pitié-Salpêtrière Hospital, France) [1]. Among the top 5 risk factors for bladder cancer queried, tobacco was ranked last by the French population. The results highlight a number of misconceptions and a lack of understanding of bladder cancer, the severity of the disease, and most importantly, tobacco is not recognised as the primary risk factor. The authors’ findings highlight the need for tailored education campaigns in the mass media all over Europe.
Dr Wei Shen Tan (University College London, United Kingdom) presented results from the DETECT 1 cohort examining a haematuria cancer risk score (HCRS) developed using 3,539 prospectively recruited bladder cancer patients from 40 UK hospitals and a validation cohort comprised of 656 Swiss patients. A lack of consensus exists regarding type of haematuria and age-specific thresholds used to guide referral for investigation of haematuria. All patients were referred to hospital for the evaluation of macroscopic and microscopic haematuria. Patient age, gender, type of haematuria, and smoking history were used to develop the haematuria cancer risk score, which detected 11.4% (n=8) more cancers which would have been missed by UK National Institute for Health and Clinical Excellence guidelines. The American Urological Association guidelines would have identified all cancers with a specificity of 12.6% compared to the 30.5% achieved by the HCRS. All patients with upper tract cancers would have been identified; these results were just recently published [2].
In short, the HCRS offers good discriminatory accuracy which is superior to existing guidelines. There is no current public health screening protocol for bladder cancer, so this study is potentially high impact. The simplicity of the model would facilitate adoption and improve shared decision-making (see Figure 1).
Figure 1: Haematuria cancer risk score in males [2]

Initiated by the EAU Guidelines panel for non-muscle invasive bladder cancer (NMIBC), there was a presentation by Dr Bas van Rhijn (Antoni van Leeuwenhoek Cancer Center, the Netherlands) comparing the prognostic value of the two classification systems for Grade determination of NMIBC. The EAU Guidelines uses both the WHO1973 (G1/G2/G3) & WHO2004/16 (low/high grade), whereas the American Urological Association Guidelines only uses the WHO2004/2016 (see Figure 2). The panel went back to patient data from 5,049 primary (first diagnosis) Ta/1 NMIBC patients from 17 centres of excellence. Both grading systems were equally capable at predicting progression, disease-specific survival, and overall survival, but not recurrence. The greatest prognostic value was seen to use a combination of WHO1973 and 2004/16. The EAU NMIBC Guideline Panel recommendation is to use both WHO systems, so be sure to ask your pathologist for both readouts.
Figure 2: NMIBC Grade classification systems
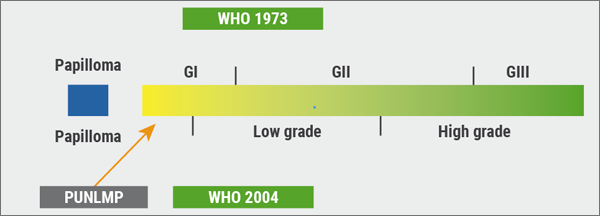
Kindly provided by Dr van Rhijn
Dr Francesco Soria (Azienda Ospedaliera Città della Salute e della Scienza di Torino, Italy) presented an interesting multicentre study (n=291) interrogating the predictive factors for the absence of residual disease at repeated transurethral resection of bladder tumour (TURBT) technique, which involves the laser resection and the wire loop resection. The primary research question was whether it is possible to avoid repeating TURBT in selected patients. All patients included had undergone an exhaustive and complete resection of a pT1 high-grade tumour, with absence of tumour at the time of second-look. Muscle was observed in 70% of pathological examinations at the first TURBT. In a multivariate analysis, the following predictive factors were identified: (1) muscle in the specimen from the beginning (HR 2.14, P=0.01); (2) concomitant carcinoma in situ (HR 0.23, P=0.002); and (3) en-bloc TURBT (HR 9.68, P=0.04). These data are being implemented into a predictive tool to aid the decision of how a patient can best be treated; there is room to challenge the second look as advocated in the guidelines.
- De La Motte Rouge T et al. J Clin Oncol 2018 36:15_suppl, 1557-1557.
- Tan WS et al. J Intern Med. 2019 Apr;285(4):436-445.
Posted on
Previous Article
« Male infertility/Premature ejaculation Next Article
What is the clinical benefit of treatment of patients with early breast cancer? »
« Male infertility/Premature ejaculation Next Article
What is the clinical benefit of treatment of patients with early breast cancer? »
Table of Contents: EAU 2019
Featured articles
Prostate Cancer
Barentsz Trial – Bi-parametric MRI versus multi-parametric MRI
Enzalutamide plus ADT improves outcomes for metastatic hormone-sensitive prostate cancer
Prostate cancer active surveillance: Better patient risk stratification and use of imaging
The role of pelvic lymph node dissection in prostate cancer: Extended vs standard
When to use imaging and imaging-guided therapies
Radioguided surgery is the future?
Bladder Cancer
Largest safety study of its kind with atezolizumab in metastatic bladder cancer
Bladder cancer risk and early detection
Consensus treatment pathway for patients with limited pelvic lymph node involvement in otherwise localised bladder cancer
FGFR3 gene mutation: Favourable prognostic impact in bladder cancer
Bladder cancer in young patients
Spanish study directly links surgical volume with mortality in bladder cancer patients undergoing cystectomy
Updated interim results of phase 2 trial of pembrolizumab for high-risk NMIBC unresponsive to BCG
Robot-assisted radical cystectomy or open radical cystectomy?
Renal Transplantation and Renal Cell Carcinoma
Andrology
Microdissection testicular sperm extraction (microTESE)
Male infertility/Premature ejaculation
Testosterone replacement therapy: Safe and maybe even protective
Focus on treatment of erectile dysfunction and Peyronie’s disease
Penile prosthesis implantation
Functional Urology
Decision aids are too difficult for patients
Lower Urinary Tract Symptoms
The Urodynamics for Prostate Surgery Trial
Minimally invasive surgical techniques must compete against pharmacotherapy in benign prostate hyperplasia (BPH)
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy


