https://doi.org/10.55788/b7b06db8
As the diagnosis of psoriasis often precedes the incidence of PsA, the potential of psoriasis treatments in delaying or preventing PsA was at the centre of the research by Ms Kathleen Miao (Keck School of Medicine of USC, CA, USA) and her colleagues [1,2]. Their retrospective cohort study strove to explore whether treatment with biologics would influence the incidence of PsA in patients with moderate-to-severe psoriasis compared with those receiving phototherapy [1]. The researchers analysed data from 4,695 patients with psoriasis from Optum’s de-identified Clinformatics® Data Mart Database between 2007 and 2021. All patients included in the study cohort received phototherapy as an index treatment for psoriasis; 461 later switched to biologics. The incidence of PsA after 10 years was defined as an outcome measure.
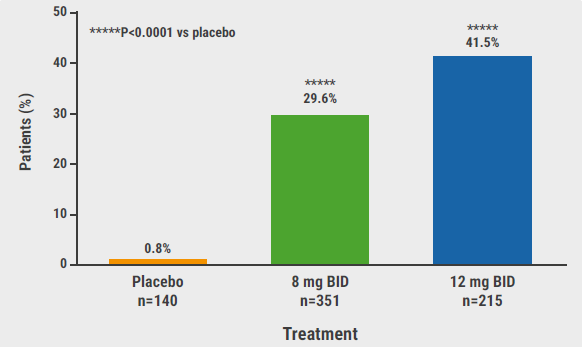
At diagnosis, the patients changing to biologics were younger (44.9 years) compared with the phototherapy patients (53.8 years). Over half of the cohort were women. PsA occurred at an incidence of 46.2 per 1,000 person-years in the entire group. Distinguished by treatment, this incidence changed to 50.0 per 1,000 person-years in the phototherapy arm and 24.6 per 1,000 person-years in the biologics arm (see Figure). With a difference of -25.48 cases of PsA per 1,000 person-years, this corresponded to a significantly lower incidence in the biologics group (P=0.0011). The hazard ratio of biologic versus phototherapy, identified by means of a Cox regression that adjusted for age, sex, and time on oral systemics, was 0.476 (P=0.005).
Figure: Intensive early therapy can reduce the cumulative incidence of psoriatic arthritis [1]

In their conclusion, the researchers suggest that biologics may reduce the incidence of PsA among psoriasis patients. To evaluate the protective extent of biologic treatment further, prospective and randomised-controlled trials are indicated.
- Miao KL, et al. Do Biologics for Psoriasis Prevent the Development of Psoriatic Arthritis? A population-based study. P42744, AAD 2023 Annual Meeting, 17–21 March, New Orleans, USA.
- Mease PJ, Armstrong AW. Drugs. 2014;74:423–41.
Posted on
Previous Article
« JAK inhibitor deuruxolitinib shows encouraging hair re-growth in alopecia areata Next Article
Bubbles and Bladder Cancer »
« JAK inhibitor deuruxolitinib shows encouraging hair re-growth in alopecia areata Next Article
Bubbles and Bladder Cancer »
Table of Contents: AAD 2023
Featured articles
New Developments in Dermatology
Delgocitinib shows promise as topical therapy for chronic hand eczema
Vitiligo patients maintain re-pigmentation after ruxolitinib cream withdrawal
Nemolizumab decreases lesions and itch in prurigo nodularis
Lichen planus: a future indication for baricitinib?
Atopic Dermatitis: State of the Art
As-needed ruxolitinib shows successful long-term symptom control in AD
Dupilumab: a viable option for atopic hand and foot eczema
Topical roflumilast beneficial in atopic dermatitis
IL-22 receptor blocker reduces itch and skin lesions in AD
Psoriasis: New Developments
Switching to risankizumab successful in IL-17 inhibitor non-responders
Novel, selective TYK2 inhibitor shows promise for psoriasis
Hidradenitis Suppurativa: What You Need to Know
Izokibep shows remarkably high grades of clinical response in HS
Bimekizumab could be the new up-and-comer for HS treatment
Pearls of the Posters
Biologics in psoriasis: can they prevent joint involvement?
JAK inhibitor deuruxolitinib shows encouraging hair re-growth in alopecia areata
Biomarkers predicting response of different CSU treatments in children
Related Articles
May 15, 2023
Topical roflumilast beneficial in atopic dermatitis

April 4, 2023
AAD 2023 Highlights Podcast
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

