The rationale of haemodynamic-guided HF management is that the addition of information about pulmonary artery pressure to clinical signs and symptoms may allow for improved HF management as elevated or increasing pulmonary artery pressure predicts congestion [1]. The multicentre, single-blind, prospective GUIDE-HF (NCT03387813) trial assessed this approach in 1,022 patients in Canada and the USA with NYHA class II–IV HF and either a hospitalisation for HF within the preceding 12 months or elevated natriuretic peptides (i.e. B-type natriuretic peptide/N-terminal pro-B-type natriuretic peptide) within 30 days. Prof. JoAnn Lindenfeld (Vanderbilt University Medical Center, TN, USA) presented the findings, which were simultaneously published in The Lancet [2,3].
All participants underwent implantation of the wireless haemodynamic monitoring device (CardioMEMS). Previously, this device demonstrated a 28% reduction of HF hospitalisations in NYHA III patients in the CHAMPION trial (NCT00531661) [4]. In the GUIDE-HF trial, patients were then randomised 1:1 to either a treatment group, managed with provider remote access to the haemodynamic data, or a control group, managed without provider access to these data. The primary endpoint was a composite of cumulative HF hospitalisations, urgent HF visits, and mortality during a median follow-up of 11.7 months.
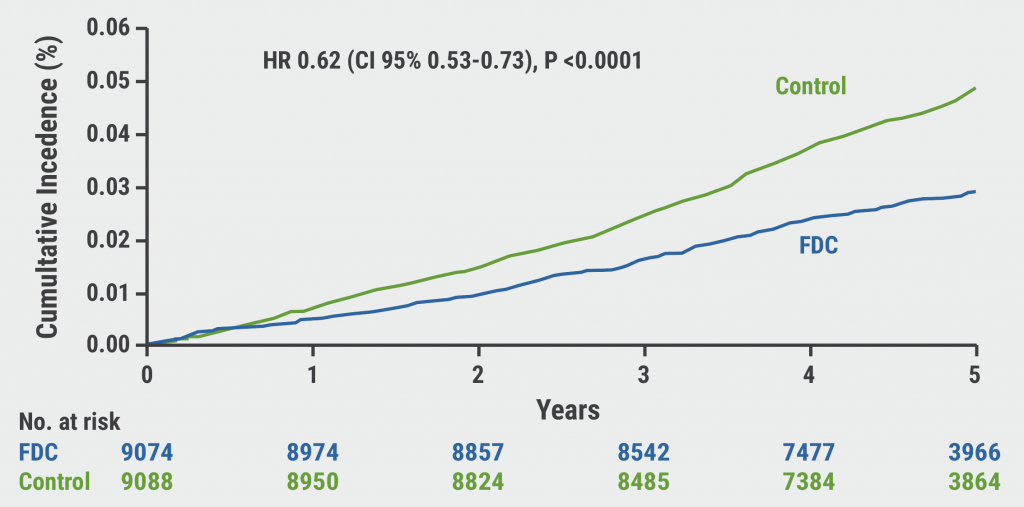
There were 253 primary endpoint events among 497 patients in the haemodynamic-guided management group and 289 in 503 patients in the control group. In the overall analysis, the primary endpoint was reduced by 12% in the treatment group. This difference failed to meet statistical significance (HR 0.88; 95% CI 0.74–1.05; P=0.16).
Interestingly, a pre-specified COVID-19 sensitivity analysis including the primary endpoint up to 13 March 2020 (the date of the national COVID emergency declaration in the USA) showed a different result: 177 primary events occurred in the intervention group and 224 events in the control group. This translated into a 19% reduction in primary endpoint events in the treatment group (HR 0.81; CI 0.66–1.00; P=0.049). This difference in primary events almost disappeared during COVID-19, with a 21% decrease in the control group relative to pre-COVID-19, virtually no change in the treatment group, and no difference between groups (HR 1.11; 95% CI 0.80–1.55; P=0.53). Again, HF hospitalisations were not reduced by haemodynamic-guided management (HR 0.83; 95% CI 0.68–1.01; P=0.064) in the overall study analysis but were lower in the pre-COVID-19 impact analysis (HR 0.72; 95% CI 0.57–0.92; P=0.007). Neither urgent HF visits nor mortality were reduced independently with treatment in the overall or pre-COVID-19 analyses. “This was a very safe device,” Prof. Lindenfeld said. Of the 1,022 participants, 1,014 (99%) had freedom from device- or system-related complications.
“The results suggest that the benefits of haemodynamic-guided management in reducing HF hospitalisations extend to patients with NYHA class II symptoms and to those with elevated natriuretic peptides, independent of prior HF hospitalisations in all ejection fractions. The COVID-19 pandemic clearly affected the outcomes of GUIDE-HF,” Prof. Lindenfeld concluded; however, given the overall neutral finding, additional studies are needed to clarify the utility of this approach.
- Abraham WT, Perl L. J Am Coll Cardiol 2017;70:389–398.
- Lindenfeld J. GUIDE-HF: haemodynamic-guided management of heart failure – randomised arm primary outcomes. Hot Line Session, ESC Congress, 27–30 August.
- Lindenfeld J, et al. Lancet 2021;398:991–1001.
- Abraham WT, et al. Lancet 2016;387:453–461.
Copyright ©2021 Medicom Medical Publishers
Posted on
Previous Article
« Cardiac arrest without ST-elevation: instant angiogram does not improve mortality Next Article
Empagliflozin: First drug with clear benefit in HFpEF patients »
« Cardiac arrest without ST-elevation: instant angiogram does not improve mortality Next Article
Empagliflozin: First drug with clear benefit in HFpEF patients »
Table of Contents: ESC 2021
Featured articles
2021 ESC Clinical Practice Guidelines
2021 ESC Guidelines on Heart Failure
2021 ESC/EACTS Guidelines on Valvular Heart Disease
2021 ESC Guidelines on Cardiac Pacing and Cardiac Resynchronisation Therapy
2021 ESC Guidelines on Cardiovascular Disease Prevention
Best of the Hotline Sessions
Empagliflozin: First drug with clear benefit in HFpEF patients
CardioMEMS: neutral outcome but possible benefit prior to COVID-19
Cardiac arrest without ST-elevation: instant angiogram does not improve mortality
Older hypertensive patients benefit from intensive blood pressure control
Antagonising the mineralocorticoid receptor beneficial for patients with diabetes and CKD
Late-Breaking Science in Heart Failure
Valsartan seems to attenuate hypertrophic cardiomyopathy progression
Dapagliflozin reduces incidence of sudden death in HFrEF patients
Late-Breaking Science in Hypertension
Smartphone app improves BP control independent of age, sex, and BMI
QUARTET demonstrates that simplicity is key in BP control
Salt substitutes: a successful strategy to improve blood pressure
Late-Breaking Science in Prevention
NATURE-PCSK9: Vaccine-like strategy successful in lowering CV events
Polypill: A successful tool in primary prevention
Important Results in Special Populations
VOYAGER PAD: Fragile or diabetic patients also benefit from rivaroxaban
COVID-19 and the Heart
Rivaroxaban improves clinical outcomes in discharged COVID-19 patients
COVID-19: Thromboembolic risk reduction with therapeutic heparin dosing
Long COVID symptoms – Is ongoing cardiac damage the culprit?
ESC Spotlight of the Year 2021: Sudden Cardiac Death
Breathing problems: the most frequently reported symptom before cardiac arrest
Lay responders can improve survival in out-of-hospital cardiac arrest
Related Articles

October 26, 2021
Empagliflozin: First drug with clear benefit in HFpEF patients
October 26, 2021
Polypill: A successful tool in primary prevention
October 26, 2021
QUARTET demonstrates that simplicity is key in BP control
© 2024 Medicom Medical Publishers. All rights reserved. Terms and Conditions | Privacy Policy
HEAD OFFICE
Laarderhoogtweg 25
1101 EB Amsterdam
The Netherlands
T: +31 85 4012 560
E: publishers@medicom-publishers.com

